
Important things You Should know about Melanoma according to a Dermatology Consultant
Melanoma is a potentially deadly form of skin cancer that can develop from normal-appearing skin. While it is important to be aware of the risks and symptoms associated with melanoma, it is also important to know that there are things you can do to reduce your risk of developing the disease. In this blog post, we will discuss some of the most important things you should know about melanoma according to a dermatologist. We hope this information helps you stay informed and proactive about your health.
What is Melanoma?
Melanoma is the most serious type of skin cancer. It arises from the cells in one’s skin that produce pigment called melanocytes. It can arise from normal looking skin or more rarely from an existing mole or birthmark. Melanoma often starts as a small, dark spot and rarely flesh colored on the skin; however, it can grow and spread quickly.
Melanoma is more common in people with light skin and hair, but can occur in all racial groups. It is associated with a history of excessive sun exposure, especially with history of sunburns and or, use of a sun tanning bed. The relationship with sun exposure is complex as melanoma can arise from non sun unexposed skin and sun exposed skin. It can occur on any part of the body, more commonly on the trunk in men and legs in women with more sinister outcomes if they occur on the face and neck.
If you notice any new skin spot which is changing in the size, shape, or color or its itching or bleeding, see your doctor right away. Early detection and treatment are important for preventing the cancer from spreading. Treatment may include surgery, radiation therapy, or chemotherapy.
If the melanoma is found before it spreads, your prognosis is good.
Lentigo maligna melanoma can affect people of all skin types, but it’s more common in light-skinned individuals who have spent a lot of time in the sun without wearing sunscreen or protective clothing. It often begins as a dark spot on the skin that may appear normal or harmless. Lentigo maligna melanoma usually begins on facial areas exposed to the sun, such as around the eyes and cheeks, forehead, nose, lips and ears. However, melanomas can start in other unlikely places too like old scars or moles anywhere on your body including your genital regions .
If you have any symptoms of melanoma, such as a change in the size, shape, or color of a spot on your skin, see your doctor right away. Early detection and treatment are important for preventing the cancer from spreading. Treatment may include surgery, radiation therapy, or chemotherapy. If the melanoma is found before it spreads, your prognosis is good.
How serious is malignant melanoma?
Malignant melanoma is a life-threatening form of skin cancer. It can be effectively treated if it is caught early, but melanoma becomes more difficult to treat as it spreads to other parts of the body. The prognosis for malignant melanoma depends on several factors, including the stage of the melanoma and the patient’s age and health at diagnosis. However, melanoma is one of the most treatable forms of cancer if it is caught early. With treatment, melanoma has an average five-year survival rate close to 95 percent. If melanoma has metastasized, the average five-year survival rate drops closer to 20 percent.
What does Melanoma look like?
Typically melanomas start as flat lesions (often called “nests”) with an irregular shape and uneven borders which are not attached to surrounding skin tissue. They can vary in color from pink, tan, brown or black depending on the amount of melanin . The majority are black brown; these colors come from melanin and melanocyte cells. Melanoma can also be skin-colored, red or purple .

Melanomas usually develop from a melanocytic nevus (plural: melanocytic naevi), which is a normal mole. However, melanomas often arise in locations where there are no moles or melanocytes present at birth such as the palms of the hands and soles of the feet. Most melanomas occur on the skin but they may rarely occur within mucous membranes . Its appearance at its early stages can be very subtle to notice, initially appearing as an increase of pale, light colored skin pigmentation without any obvious shape or border. It may later grow into larger dark brown/black patches with irregular borders.
The lesion may also be accompanied by other symptoms, such as itching, bleeding, or pain. If melanoma is not treated, it can metastasize (spread) to other parts of the body, which may result in death. melanoma cause is unknown but it has been linked with exposure to ultraviolet radiation from sunlight or tanning lamps/beds, a history of sunburns, and certain genetic factors. melanoma treatment naturally depends on the stage of melanoma.
As melanoma cells grow, they may spread (metastasize) to other parts of the body. The melanoma may spread to lymph nodes near the site of the tumor or it may spread to other organs such as the lungs, brain, or liver.
Where is Melanoma usually found
Melanomas usually occur on areas like the back (lower part), torso (front and back), head/neck , legs, arms, face (nose, lips) and genitalia . People who spend time outside are at greater risk for developing melanomas because melanin makes skin darker to absorb more UV rays. Sun-exposed areas include the lower part of the back, legs, arms and face (nose, lips, ears).
Melanoma in the nails
It is a rare type of melanoma, accounting for less than 1% of all melanomas. Melanoma in the nails can occur in any nail, but is most common in the toenails.
The cause of melanoma in the nails is not known, but it is likely due to a combination of genetics and environmental factors. The early signs of melanoma in the nails are often overlooked, as they can be mistaken for a fungal infection or other benign condition. As melanoma in the nails grows, it can cause the nail to thicken, change color, or split.
Melanoma on the scalp
Melanoma on the scalp is melanoma that forms in melanocytes in the skin of your scalp. This type of melanoma isn’t as common as melanoma on other parts of the body, but it can be very serious if you don’t treat it.
Symptoms of melanoma on the scalp include a mole or lesion on the scalp that changes in size, shape, or color. If you notice any changes in a mole on your scalp—or have any other symptoms of melanoma—see a doctor right away.
Treatment for this type of melanoma is largely based on where your melanoma is diagnosed and how thick it is. Treatment options include surgery to remove the cancerous cells, radiation therapy, and immunotherapy.
Melanoma in the toenail
Melanoma that occurs in the nails can look different depending on where it is located. melanoma that occurs in the toenail often looks like a black or brown streak under the toenail. Melanoma that occurs in the fingernail often looks like a black or brown dot on the surface of the nail.
Melanoma that occurs in the nails can be difficult to diagnose because it may not cause any symptoms. melanoma in the nails is often found in a person’s routine dermatological examination. Sometimes, melanoma can bleed or become infected, which leads to a foul smell from the area of the melanoma .
Melanoma that occurs in the toes and feet is more aggressive than melanoma that occurs anywhere else on the body. This makes melanoma that occurs under a toenail more likely to spread through lymph vessels or blood stream to other parts of the body, such as nearby lymph nodes and other nearby tissues and organs .
Melanoma versus carcinoma
Melanoma and carcinoma are both types of skin cancer, but melanoma is a more serious type of skin cancer. melanoma starts in melanocytes, which are the cells that produce melanin, while carcinomas start in other types of cells. Carcinomas are more common than melanomas, and they can spread to other parts of the body. melanomas are less likely to spread, but they can be more aggressive and harder to treat.
There are several ways to tell the difference between melanoma and carcinoma:
- Melanomas tend to have a black or brown color, while carcinomas are usually red or white
- Melanomas often have an irregular shape, carcinomas are more likely to be round
- Melanomas are more likely to grow on the skin, while carcinomas are more likely to grow in internal organs
Grading Melanoma
Grading melanoma is an important part of assessing the severity of the cancer. The grading system takes into account how deeply the melanoma has penetrated the skin, as well as the tumor’s size and shape. A higher grade melanoma means that the cancer is more aggressive and may be more likely to spread. There are five grades of melanoma, with Grade 1 being the least severe and Grade 5 being the most severe.
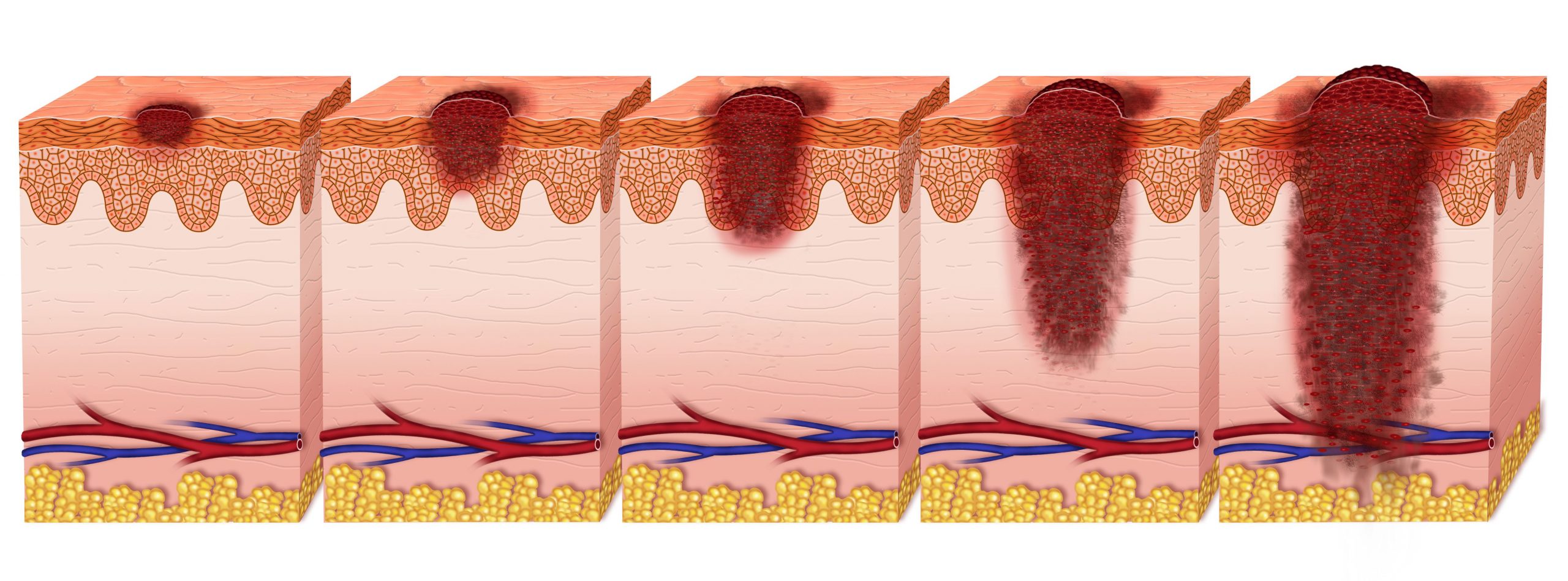
The grading system for melanoma is as follows:
Grade 1
Melanoma is a small, thin tumor that has not penetrated below the surface of the skin.
Grade 2
Melanoma is a thicker tumor that has not penetrated below the surface of the skin.
Grade 3
Melanoma is a thicker tumor that has penetrated below the surface of the skin.
Grade 4
Melanoma is a very thick tumor that has penetrated below the surface of the skin.
Grade 5
Melanoma is a very thick tumor with cells that have spread to other parts of the body.
What are the stages of melanoma?
Staging melanoma is the most accurate predictor of prognosis. The lower the melanoma stage, the higher the chance of cure. In order to determine melanoma staging, a pathologist cuts and stitches together multi-layered sections from a melanoma sample to see how deeply the melanoma has invaded skin tissue.
Pathologists assign each block specimen a clinical issue number according to its characteristics under a microscope, then they send it to a central pathology lab for analysis.
1) Benign cellular changes – No melanomas or only benign nevi (lentigo maligna melanomas, melanomas in situ)
2) Mild melanocytic proliferation – Atypical melanocytic nevi or melanoma in situ
3) Moderate melanocytic proliferation – Moderately dysplastic nevi or melanomas in situ with tumor nests up to 0.5mm deep
4) Severe melanocytic proliferation – Moderately dysplastic nevi or melanomas in situ with tumor nests greater than 0.5mm deep, deeply invasive melanomas, and melanoma metastasis.
Pathologists also use a staging system for melanoma that reflects how much the tumor has spread. There are five stages of melanoma:has five stages; Stage I, Stage II, Stage III, Stage IVA and Stage IVB. Each stage serves as a predictor of metastasis and survival rates.
The lower melanoma stage, the higher chance of cure.
Staging for melanoma is as follows:
Stage I
Tumors are small and have not spread beyond the original site (in situ).
Stage II
Tumors are larger than Stage I melanomas, but have not spread to the lymph nodes or other parts of the body.
Stage III
Melanomas have spread to the lymph nodes, but not to other parts of the body.
Stage IV
Melanomas have spread beyond the lymph nodes to other parts of the body.
What stage of melanoma is bad?
Melanoma can be divided into five stages, with stage IV being the most advanced. Melanoma in stage IV has a poor prognosis, with a five-year survival rate of less than 20%. The earlier melanoma is caught, the better the prognosis. For example, the five-year survival rate for melanoma in stage I is nearly 100%.
If melanoma is caught in stage II, the five-year survival rate is about 70%. If melanoma is caught in stage III, the five-year survival rate is about 50%. If melanoma has spread to regional lymph nodes, the five-year survival rate drops to about 30%. And if melanoma has spread to distant organs, the five-year survival rate is only about 10%.
It’s important to remember that these are just averages. Everyone’s melanoma will be different, and your individual prognosis will depend on a number of factors, including your age and overall health, the size and location of the melanoma, and how aggressive it appears.
If you have been diagnosed with melanoma, it is important to talk to your doctor about what stage your melanoma is and what treatment options are available to you. Treatment options vary depending on the stage of melanoma. Stage IV melanoma may require more aggressive treatment, such as chemotherapy or radiation therapy.
Why does Melanoma spread so fast?
There are several ways melanoma can spread. It can break away from the original tumor and travel through the bloodstream or lymphatic system to other parts of the body. melanoma can also spread to nearby tissues or organs.
One of the reasons melanoma spreads so fast is that it can evade the body’s immune system. The cancer cells may produce proteins that disguise them from the immune system or suppress the immune system’s ability to fight cancer.
Another reason why melanoma spreads quickly is that it can invade blood vessels and travel through them to other parts of the body.
Additionally, melanoma spreads quickly is because it can metastasize, or spread, to other parts of the body. Metastasis is the process by which cancer cells break away from the original tumor and travel to other parts of the body.
There are several factors that contribute to melanoma’s ability to metastasize. One factor is that melanoma can spread through the bloodstream and lymphatic system. Another factor is that melanoma can invade blood vessels and travel through them to other parts of the body.
In addition, melanoma cells can release enzymes that help them invade surrounding tissues. These enzymes can damage nearby tissues and organs, making it easier for melanoma to spread.
Another reason melanoma spreads so quickly is that melanoma cells produce proteins that disguise them from the immune system or suppress the immune system’s ability to fight cancer. In this way melanoma can trick the body into ignoring it. melanomas lack of recognition by the body’s immune defenses plays a major role in why melanomas are likely to grow and may be life-threatening when they metastasize.
It is important to remember, however, that melanoma cells can adapt and evolve over time – making each melanoma different from every other one. Because of this, no two melanomas behave exactly alike or respond to treatments in the same way. The factors listed above contribute largely to melanomas ability to spread, but each melanoma is unique and will display different characteristics.
What is the survival rate of malignant Melanoma?
The survival rate of melanoma varies depending on the stage of the cancer. In general, the five-year survival rate for melanoma is around 85%. However, the prognosis for melanoma is much better when it is caught early. If melanoma is caught before it has spread to other parts of the body, the five-year survival rate jumps up to 95%. Unfortunately, if melanoma has already spread to other parts of the body, the five-year survival rate falls to around 15%.
There are a number of different factors that can affect a person’s prognosis with melanoma. Some of these factors include:
- The thickness of the melanoma tumor
- The location of the melanoma tumor
- The stage of the melanoma tumor
- The age of the person with melanoma
- Whether or not the melanoma has spread to other parts of the body
What is the life expectancy of someone with metastatic Melanoma?
The life expectancy of someone with metastatic melanoma varies depending on a number of factors including age, gender, and the stage of melanoma at initial diagnosis. The median overall survival for patients diagnosed with melanoma that has metastasized is 11-19 months from time of diagnosis however there are still “about 10% to 15% [of these patients] who survive five years or longer.”
In addition to age and melanoma stage, other factors found to affect prognosis in melanoma include: tumor thickness and presence of ulceration. Tumor thickness is significantly associated with both survival and metastasis, so it’s essential for individuals diagnosed with melanoma, or melanomas whose thickness can not be assessed because of small sample size, to closely follow treatment plans in order to prevent the tumor’s thickness from increasing.
Despite the fact that melanoma is a serious cancer, there are treatments available that can improve a person’s prognosis. Treatment options include surgery, chemotherapy, and radiation therapy. In some cases, a combination of these treatments may be used. It is important to remember that each case of melanoma is unique and should be discussed with a doctor to get a personalized treatment plan.
Can Melanoma be cured?
Yes.
The melanoma cure rate for those who catch it early is at least 90%, melanoma can often be cured by removing it through surgery. Sometimes melanoma may recur even after removal – this means that there were some microscopic cancer cells left behind which grew into new tumors later on. Although melanomas can be cured by removing them surgically, melanoma surgery carries the risk of removing healthy tissue along with melanoma cells.
The melanoma cure rate once melanoma has spread to other parts of the body is very low, though melanomas are sometimes still curable by surgical removal if discovered early.
What is the latest treatment on Melanoma
Some new treatments for melanoma include:
Immunotherapy
Immunotherapy uses drugs or other substances to boost the body’s natural defenses to fight cancer. Immunotherapy can be used alone or in combination with other treatments. Some of the immunotherapy drugs used to treat melanoma include nivolumab (Opdivo) and pembrolizumab (Keytruda).
BRAF inhibitors
Some melanomas have a mutation in the BRAF gene. Drugs that block the action of this gene, called BRAF inhibitors, can be effective in treating melanoma. The most common BRAF inhibitors used to treat melanoma are vemurafenib (Zelboraf) and dabrafenib (Tafinlar).
Targeted therapy
Drugs that target specific molecules involved in cancer growth can be effective in treating melanoma. Some of the targeted drugs used to treat melanoma include trametinib (Mekin) and cobimetinib (Cotellic).
Dabrafenib & Trametinib
Researchers are also exploring the use of dabrafenib and trametinib to treat melanoma. This treatment was approved by the Food and Drug Administration (FDA) in 2014.
Combination therapy
Immunotherapy drugs, BRAF inhibitors, or both, are most often used in combination with other melanoma treatments. For example, these treatments may be given together with targeted therapy if melanoma cells have a mutation that makes melanomas more sensitive to treatment with these drugs.
Surgery
Melanoma is usually treated with surgery to remove the melanoma, followed by treatment with immunotherapy or targeted therapy, if needed. If melanomas are widespread throughout the body, they may be treated with immunotherapy alone after surgery. This treatment is called adjuvant melanoma therapy.
Most people have melanomas removed immediately because melanomas can develop quickly and spread to other parts of the body within weeks or months. An exception is when melanomas are large but do not appear to have spread beyond where they started developing in the skin (called stage 0 melanoma). In these cases, doctors often recommend waiting 6 weeks between tests to see whether melanomas are starting to grow into nearby tissue.
Treatment for stage 0 cancers that still look like melanomas at the 6-week follow-up is most often surgery to remove the melanoma. However, some people with stage 0 melanomas may choose to have no treatment or to wait and see if the melanoma disappears on its own.
Conclusion
Melanoma is a very common, but also dangerous form of skin cancer. Early diagnosis and treatment can save your life with the right therapy plan. We hope this publication has given you the industry insight into the best course of action for skin cancer treatments, that are the gold standard according to various board-certified skin specialists.
If you are worried about being able to spot this fatal disease on your own body or want to learn more about different treatments that might work best for you, click here to select Dr. Nico Mousdicas, MD as your Personal Concierge Dermatologist.

BLOG AUTHOR
Dr. Ismail Sayeed
Dr. Sayeed is the Medical Director of ViOS, Inc. He is a deeply committed physician entrepreneur & medical blog writer. While building the global infrastructure of the VIOS Clinic, he is dedicated to educate people on the potential of specialist telemedicine for managing chronic diseases.
Read more about him in his author bio







0 Comments